This article explores how rheumatology contributes to long-term quality of life for people managing chronic joint or autoimmune conditions, and this opening sentence stays between one hundred forty and one hundred sixty characters to ensure an effective and SEO-friendly meta description as you requested.
Why Do Chronic Joint Symptoms Affect Daily Life So Deeply?
People often underestimate how much persistent joint stiffness or pain influences even the simplest moments of the day. A morning routine that once felt effortless can suddenly demand more patience and energy than expected. According to our editor’s research, many individuals describe these symptoms as “small interruptions that slowly grow louder,” affecting mood and mobility over time. When discomfort becomes repetitive, it reshapes how people plan their schedules and interact socially. These subtle adjustments accumulate and gradually weaken the sense of control people feel over their wellbeing. Understanding this emotional dimension helps explain why rheumatology plays such a vital role in long-term quality of life.
What Makes Rheumatology Different from General Care?
Rheumatology focuses on conditions that often blend inflammation, immune activity, and structural changes in the joints. This combination creates a unique health puzzle requiring careful observation. Many patients arrive at a rheumatology clinic after months of subtle symptoms that never fully resolve. As a result of our editor’s reviews, individuals often express relief when finally meeting a specialist who recognizes patterns that general evaluations may overlook. Rheumatologists assess not only symptoms but also how those symptoms change throughout the day. This deeper approach helps identify conditions that evolve slowly but influence long-term wellbeing. With the right guidance, people gain clarity and begin understanding their body’s signals more confidently.
How Does Early Diagnosis Shape Long-Term Outcomes?
Early diagnosis allows people to address inflammation before it causes wider structural changes. Many joint-related conditions begin with mild stiffness or occasional swelling that feels harmless at first. According to our editor’s research, patients often delay seeking help because the discomfort comes and goes unpredictably. Yet these early phases offer a valuable opportunity to reduce long-term complications. Early intervention improves physical comfort and preserves joint mobility. When people act before the inflammation becomes chronic, they create a protective barrier around their long-term wellbeing. Understanding these early signs empowers people to take the right steps rather than waiting for symptoms to worsen.
Why Are Autoimmune Conditions Often Misunderstood?
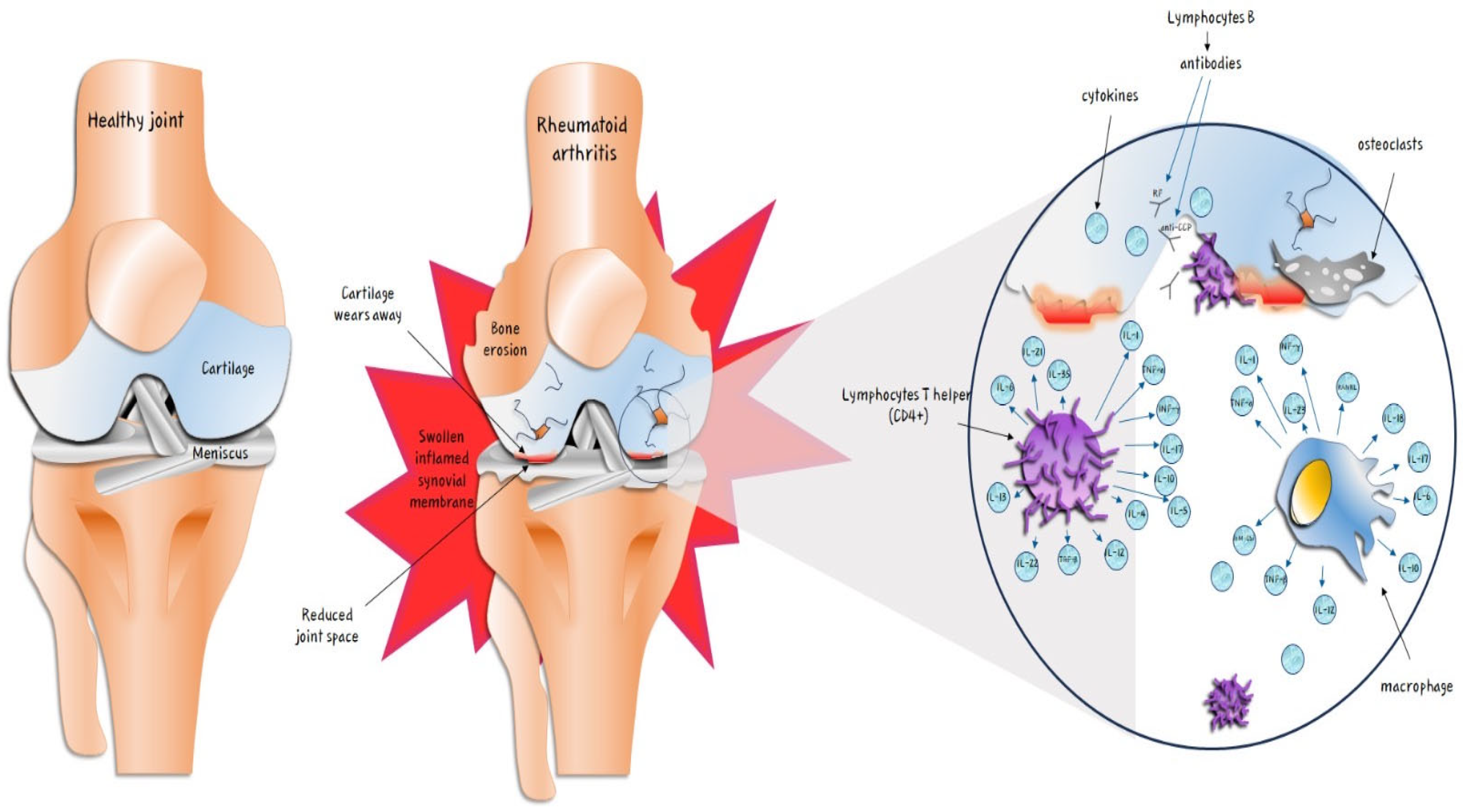
Autoimmune diseases can create confusing symptom patterns because the immune system behaves unpredictably. One day feels stable, while another day brings sudden flare-ups without clear triggers. As a result of our editor’s reviews, people frequently report feeling misunderstood before receiving a proper diagnosis. Friends and colleagues may not see outward signs of discomfort, making the experience feel isolating. Rheumatology bridges this understanding gap by acknowledging how invisible symptoms still impact quality of life. Conditions like rheumatoid arthritis, lupus, or ankylosing spondylitis require long-term planning rather than short-term fixes. This clarity reassures people that their experiences are real and manageable with the right approach.
What Role Does Personalized Treatment Play in Daily Comfort?
Personalized treatment helps individuals balance symptom control with daily activities. Rheumatologists often explore a combination of medications, lifestyle adjustments, and monitoring strategies. According to our editor’s research, people respond best when treatment aligns with their routine and priorities. A tailored plan reduces flares and builds predictability, which improves confidence in daily movement. Personalized care also considers emotional wellbeing, acknowledging how chronic conditions influence long-term mental balance. When individuals feel supported through customized strategies, their overall comfort grows steadily. A thoughtful treatment approach becomes a reliable partner in navigating long-term health needs.
How Does Lifestyle Influence Rheumatology Outcomes?
Lifestyle plays a meaningful role in how rheumatologic conditions behave over time. Small routines such as stretching, balanced eating, or gentle exercise contribute noticeably to daily comfort. As a result of our editor’s reviews, many people observe reduced stiffness when maintaining consistent habits. Even slight improvements in movement or posture can ease the body’s workload. Environmental factors also influence symptoms, especially during humidity changes or prolonged periods of stress. Developing supportive habits builds a healthier foundation for treatment to work effectively. These practical steps serve as tools people can control, which strengthens long-term wellbeing.
Why Does Mental Health Matter in Rheumatologic Care?
Living with chronic symptoms can create emotional strain that slowly shapes the way people interpret their experiences. Feelings of uncertainty may appear during flare-ups or moments of reduced mobility. According to our editor’s research, many individuals describe a growing sense of vulnerability if symptoms persist without understanding. Rheumatology recognizes this emotional aspect and includes mental wellbeing within the long-term care perspective. Creating a realistic, manageable routine helps reduce anxiety and strengthens resilience. When people feel emotionally supported, their physical symptoms often become easier to manage. Mental confidence reinforces quality of life in powerful ways.
How Does Ongoing Monitoring Improve Stability?
Rheumatologic conditions often change gradually, requiring steady observation rather than occasional evaluations. Regular monitoring helps identify shifts that may require treatment adjustments. As a result of our editor’s reviews, individuals feel more secure when they know their progress is tracked carefully. This ongoing relationship between patient and specialist creates a sense of shared responsibility. When monitoring becomes consistent, flare-ups become easier to predict and prevent. People gain a clearer understanding of how their body responds to stress, activity, or environmental changes. Continuous guidance strengthens long-term stability and improves daily wellbeing.
How Can People Maintain Mobility Over Time?
Mobility often becomes one of the biggest concerns for individuals managing rheumatologic conditions. Joint stiffness can limit movement and reduce confidence in physical activities. According to our editor’s research, even light daily routines influence how the body handles long-term strain. Gentle exercises like stretching or low-impact walking support joint health and ease tension. When people maintain steady movement, they protect their joints from long-term stiffness. These habits help preserve independence and prevent unnecessary discomfort. Consistent mobility practices become a form of long-term investment in quality of life.
When Should Someone Reassess Their Treatment Plan?
Treatment needs may change as symptoms evolve, making reassessment an essential part of long-term wellbeing. People sometimes feel hesitant to mention worsening symptoms, assuming it is part of the condition. As a result of our editor’s reviews, individuals benefit greatly from updating their plan when discomfort becomes more frequent. Reassessment helps prevent long-term complications and ensures medications remain effective. Rheumatologists evaluate whether new routines, changed lifestyles, or emerging symptoms require adjustments. Staying proactive ensures treatment grows alongside the person rather than falling behind the condition’s progression.
How Does Rheumatology Strengthen Long-Term Quality of Life?
Rheumatology offers a structured and compassionate approach to managing chronic symptoms, giving people long-term strategies rather than temporary relief. By combining personalized treatment, steady monitoring, and lifestyle awareness, individuals build a healthier daily routine. According to our editor’s research, people feel more in control when they understand how their body responds to different influences. Rheumatology supports this understanding and provides consistent guidance. When people feel less burdened by symptoms, their emotional balance and physical comfort improve naturally. This collaborative care empowers long-term wellbeing in meaningful ways.